Flex robot gives Sentara doctors access to hard-to-reach throat cancers.

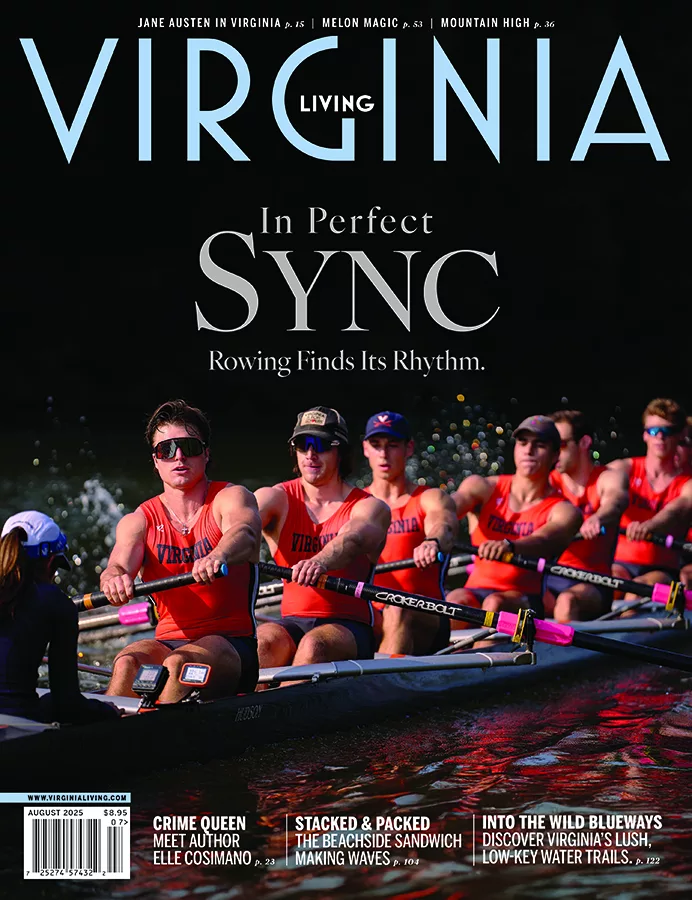
Dr. Karakla, center, and care team.
Photo courtesy of Sentara
For four months, Robert Banks, 58, had a sore throat that wouldn’t go away. “My family encouraged me to go to my primary care doctor. Even though the CT scan that he ordered did not show anything impressive, he was convinced that it was something more,” says Banks. A biopsy confirmed that the Elizabeth City, North Carolina, native had stage 1 supraglottic cancer—cancer in the upper part of the voice box and the epiglottis, the cartilage flap that opens and closes on top of the windpipe. Even though he had smoked for more than 40 years, he was surprised to learn the diagnosis. But he says, “Deep down, I knew that a sore throat for that amount of time was not ‘normal.’”
Dr. Daniel Karakla, a head and throat surgeon with Sentara Eastern Virginia Medical School Comprehensive Head and Neck Center, operated on Banks using the innovative Flex Robotic System. The technology, purchased by the center in September 2017, enabled the surgeon to remove the patient’s entire epiglottis and upper portion of the larynx without harming any healthy surrounding tissue. Featuring a highly bendable arm and flexible tools, the Flex fits into patients’ mouths better than an older and more rigid, three-armed robotic system and allows Karakla to access “areas that are more difficult to reach with traditional scope equipment, traditional tools,” he says.
Karakla uses a joystick to direct the tube down, bending around the curve of the throat. Once it arrives, he deploys tools through the tubing. The surgeon controls the long, flexible tools from outside the mouth—watching the movements on imaging provided by the unit’s tiny camera.
Years ago, patients like Banks might have required radiation therapy with or without chemotherapy or “a jaw split approach, where you make an incision on the neck, split the jaw, open it up like a book, remove the cancer, and then close things up, with or without a flap to reconstruct it,” says Karakla. “Now that we can remove tongue base and tonsil cancer by way of robotic assistance, that gives us another weapon against the cancer.”
In Banks’ case, “We were trying to avoid the need for radiation therapy in this patient, and so far it looks like we have been able to do that,” he says.
Banks’ surgery took place in March 2018. He required a tracheotomy and feeding tube initially—not unusual for this type of operation—but within a week was able to lose the feeding tube and return home to begin his recovery. His ability to speak was not affected, although he did have to re-learn to swallow. He’s now able to eat and drink again. A second surgery to remove the highest risk neck nodes revealed the cancer had not spread.
“Overall, I think my recovery went well,” says Banks. Additionally, “I have been smoke-free since my surgery—something that I never thought would happen for me. The severity of my diagnosis was far greater than [the need for] any cigarette.” Sentara.com
This article originally appeared in our December 2018 issue.